Baxter’s Neuropathy
- Whitney Lowe
Pain on the bottom surface of the foot can be a debilitating condition; in cases, persisting for several years. The most common cause of plantar foot pain is plantar fasciitis. Pain on the underside of the foot that is aggravated with activity is often diagnosed as plantar fasciitis. Yet in some cases this pain persists despite attempted treatment and does not respond to the typical treatments for plantar fasciitis. When standard treatments are unsuccessful the primary problem may not be with the plantar fascia at all.
A potential cause of plantar foot pain that can easily mimic symptoms of plantar fasciitis is compression of the inferior calcaneal nerve (ICN) under the arch of the foot. The ICN is a branch of the lateral plantar nerve on the bottom surface of the foot. The nerve is also sometimes called Baxter’s nerve, named after the first physician to describe this nerve compression as a specific cause of foot pain. Compression pathology of this nerve is therefore called Baxter’s neuropathy.
Location and Structure
The tibial nerve divides into two primary branches, the medial and lateral plantar nerves, as it passes around the medial side of the ankle in the tarsal tunnel (Figure 1). Both branches then curve around the medial ankle and course along the bottom surface of the foot.
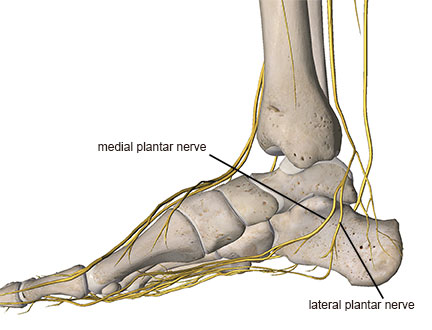
Figure 1
The first smaller branch that splits off from the lateral plantar nerve is the inferior calcaneal nerve (ICN) (Figure 2). In most people the ICN branch splits off from the lateral plantar nerve on the underside of the foot. However, in some cases the ICN may actually branch off more proximally, even as far up as the tarsal tunnel on the medial ankle.
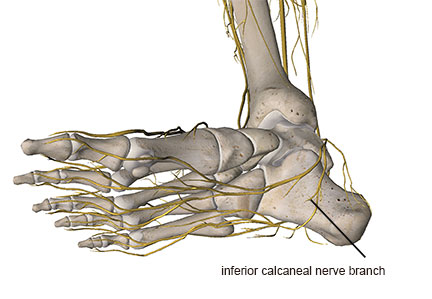
Figure 2
Where and how a nerve branches is clinically relevant because nerve branching can increase tensile or compressive loads on the nerve and lead to nerve injury.1 Another factor that makes the plantar nerves and their branches more susceptible to injury and irritation is the sharp right angle turn they take from the medial side of the foot to the plantar surface.
In Baxter’s neuropathy there are two potential locations of entrapment of the ICN. The first is between the deep fascia of the abductor hallucis muscle and the quadratus plantae muscle (Figure 3).
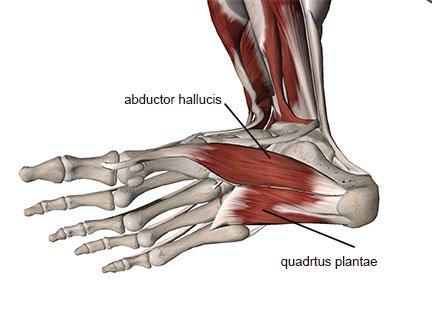
Figure 3
The second is along the medial calcaneal tuberosity where the nerve can be compressed against the bone or bone spurs that may have developed along the anterior calcaneus (Figure 4).
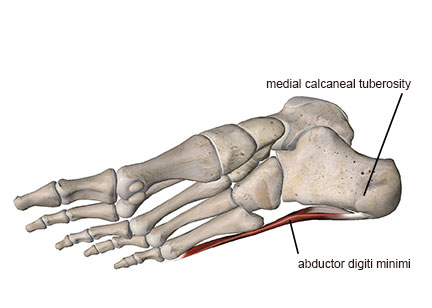
Figure 4
Bone spurs at the anterior calcaneus are assumed to result from tensile forces on the attachment sites of the toe flexor muscles or the plantar fascia. The presence of bone spurs is frequently described as a primary cause for heel or foot pain. However recent theories have suggested that while bone spurs may be a result of certain biomechanical forces in the foot, they may not be a primary cause of foot pain.
Because spurs occur on the anterior calcaneus, it is unlikely that there is pressure from weight-bearing directly on the spur. Additionally, spurs also occur in other locations in the body without being painful. It may be that in a case where bone spurs are present, ICN nerve compression is a primary cause of the pain. The spur can project into the path of the ICN and cause increased nerve compression.
Assessment
Baxter’s neuropathy may account for up to 20% of heel pain cases.2,3 A description of this condition does not occur frequently in much of the orthopedic literature, which suggests that if it is thought to be present in 20% of heel pain case then it may be being misdiagnosed. If it is misdiagnosed as another common condition such as plantar fasciitis, traditional treatments could be ineffective, or actually make the condition worse. Treatment approaches for plantar fasciitis are highly variable, so it’s wise to consider the possibility that ICN compression is a factor in any long-term complaint, especially if it does not respond to traditional treatment.
The ICN is a mixed motor and sensory nerve so nerve compression may cause pain in the foot or ankle, along with muscular atrophy if the motor fibers are affected. When motor fibers are involved, the abductor digiti minimi (ADM) muscle is the one most commonly affected although the inferior calcaneal nerve also may innervate the flexor digitorum brevis and the quadratus plantae muscles in some cases (Figure 5).
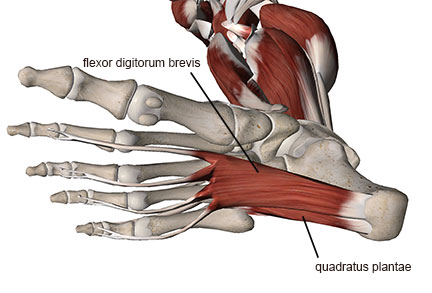
Figure 5
It is challenging to identify compression of the inferior calcaneal nerve with physical examination. However, a few methods may help determine the possibility of this nerve’s involvement. Pain elicited with palpation along the arch on the bottom surface of the foot is usually present. In some cases pain with palpation will be exaggerated along the lateral aspect of the plantar surface where the ADM muscle is located. Pain may also be elicited with palpation along the medial arch where the nerve is likely to be entrapped.
The flexor digitorum muscle is not always innervated by the inferior calcaneal nerve, but when it is there may be weakness of this muscle that is apparent with resisted flexion of the last four toes. One way to examine this is to place a thick card like a business card or standard 3X5 index card on the ground. Have the client attempt to hold the card down with all four toes as you attempt to slowly pull it out (Figure 6). If they are unable to hold the card, or it appears easier to pull the card away than when the same procedure is performed on the other side, there is likely weakness in the flexor digitorum brevis muscle. This may indicate potential compression of the inferior calcaneal nerve.

Figure 6
One of the more accurate methods of determining involvement of this small nerve is with an MRI.4
When motor fibers to the ADM muscle are damaged, the muscle will atrophy and fatty edema can build up in the muscle. The fatty infiltration of muscle is visible on the MRI. Because it is so difficult to identify the clinical indicators of inferior calcaneal nerve compression through physical examination, this nerve compression pathology is often missed if an MRI is not performed.
Baxter’s neuropathy is likely to occur in conjunction with other foot pain problems, making its presence more difficult to identify. One study found a strong correlation between ICN compression and three other key factors: increased age, calcaneal bone spurs, and plantar fasciitis.2 It may also result from certain biomechanical challenges in the foot such as pes planus (flat foot).4
Treatment Strategies
As with all nerve compression problems, it is important not to exaggerate nerve irritation with treatment, as it could make the condition worse. Communicate closely with your client as you work to make sure symptoms aren’t being significantly increased as you use these or other treatments.
Because compression of the nerve can occur between soft tissues (the deep fascia of the abductor hallucis muscle and the quadratus plantae muscle), massage could be helpful in reducing any compressive forces on the nerve. Soft tissue treatment may also be beneficial in reducing nerve irritability by reducing tensile forces pulling on the nerve.
In many cases nerve pain is increased because of tensile or compressive forces on the nerve. These forces may be relatively small but still produce detrimental results. Moving soft tissues in a direction that relieves stress on the nerve is often very helpful and allows the brain to reset its perceived noxious input from pain receptors, further decreasing pain. Knowing your anatomy is critical in order to find the appropriate direction to move the foot, which can also vary to some degree from person to person.
The massage therapist can do this by moving the foot in particular directions that relieve that tension. The first way to do this is to move the foot into inversion. Effectiveness in this treatment will be known when the direction of movement is one that relieves tensile loading on the nerve and reduces pain. Experiment with your client on what position feels best.
The second way to relieve nerve tension is accomplished by grasping the heel and hindfoot and gently pulling it in a medial direction (Figure 7). Ask the client if the position or movement reduces any of the foot pain. The ADM muscle or arch of the foot may be painful with palpation. It may be helpful to press on one of these sore areas as you perform the heel/foot movements. Look for reduced pain when this technique is applied.

Figure 7
Once you find a position that decreases pain, hold it for about two minutes and then very slowly and gradually let it go. After releasing the hold, perform very gentle and easy passive movements with the foot to help encourage a freedom of movement and to reestablish new reduced levels of neural reporting. The more frequently this technique is applied, the more beneficial it will be. It is helpful to teach the client how to do this at home. Compliance is key to successful treatment.
It is likely that you will continue to encounter clients that complain of plantar foot pain. If traditional strategies are unsuccessful, it is a good idea to consider other possibilities such as ICN compression. Many people have to live with this significant pain for a long time without anyone considering other possibilities that might be the cause. If you are that one healthcare professional that looks out of the box to help them find relief, you will be forever appreciated as this condition can be disabling.
Notes:
- Butler D. Mobilisation of the Nervous System. London: Churchill Livingstone; 1991.
- Chundru U, Liebeskind A, Seidelmann F, Fogel J, Franklin P, Beltran J. Plantar fasciitis and calcaneal spur formation are associated with abductor digiti minimi atrophy on MRI of the foot. Skeletal Radiol. 2008;37(6):505-510.
- Pecina M, Markiewitz A, Krmpotic-Nemanic J. Tunnel Syndromes: Peripheral Nerve Compression Syndromes. Boca Raton: CRC Press; 2001.
- Dirim B, Resnick D, Ozenler NK. Bilateral Baxter’s neuropathy secondary to plantar fasciitis. Med Sci Monit. 2010;16(4):CS50-CS53.

