Exploring Plantar Foot Pain
- Whitney Lowe
Introduction
Plantar foot pain can be a debilitating condition that severely impacts a client’s quality of life. There are numerous causes of foot pain, and the ideal treatment for each condition varies depending on the nature of the problem. In this post we explore several potential causes of plantar foot pain. In a future post, we’ll look at key treatment strategies based on the Ladder of Engagement treatment model.
Plantar Fasciitis
Plantar fasciitis is the most common cause of pain on the bottom surface of the foot. It is prevalent with athletes and others that spend long hours on their feet or have repetitive impact loading. The condition is also aggravated by various biomechanical factors such as a pes planus (flat foot) or pes cavus (excessively high arch).
The plantar fascia attaches proximally to the anterior calcaneus and distally blends into the ligaments surrounding the metatarsophalangeal (MTP) joints and flexor tendon sheaths of all five metatarsals (Image 1). It provides the primary soft-tissue support for the longitudinal arch.

Image courtesy of Complete Anatomy
The plantar fascia is crucial for shock absorption in the lower extremity. Reducing these impact forces is particularly important in sporting activities because ground reaction force can be 2–3 times the body’s weight when running. Without tissues such as the plantar fascia mitigating these forces, individuals could develop a host of problems such as stress fractures, joint disorders, shin splints, or other overuse conditions.
The plantar fascia functions primarily as a spring to maintain the foot’s arch. The shape of the arch can frequently determine how effective the plantar fascia’s function is. Pes planus (flat foot) has a poor longitudinal arch, which decreases the shock-absorbing capability of the plantar fascia. Pes cavus (excessive arch) may cause chronic overuse to the plantar fascia because tension increases, causing greater stress on its attachment site on the anterior calcaneus.
Plantar fasciitis is routinely considered an inflammatory condition involving the attachment site of the plantar fascia on the calcaneus. However, inflammation may not always be involved, and the primary tissue irritation could be collagen degeneration in the fascia akin to that experienced in overuse tendinosis. Both processes (inflammatory and non-inflammatory) could potentially be involved in the condition.
Fiber degeneration in the plantar fascia can occur anywhere along its course, but the primary site of involvement is the proximal attachment at the anterior calcaneus. The attachment site is particularly painful because the plantar fascia blends in with the periosteum around the calcaneus at the attachment site. The periosteum is one of the most pain-sensitive tissues in the body, so pulling on it produces significant pain. Repetitive tensile stress on the calcaneal attachment site can also cause an exostosis (bone spur) to develop. Plantar fasciitis may exist without bone spurs, and bone spurs may exist without plantar fasciitis.
Several mechanical factors play a role in the onset of plantar fasciitis. Overpronation is a recognized cause of plantar fasciitis. Ordinarily, the tibialis posterior muscle aids the plantar fascia in shock absorption. The muscle’s function is often compromised in overpronation, and the plantar fascia has to take on a more significant role in shock absorption in the lower extremity. Hypertonicity or myofascial trigger points in the triceps surae (gastrocnemius and soleus) muscles may also set up dysfunctional tension patterns in the foot muscles, which can contribute to plantar fasciitis as they limit the spring action in the foot.
A sudden change in activity levels, such as that with new military recruits, is routinely linked to plantar fasciitis. Significant weight gain, especially over a short period, may also put additional stress on the plantar fascia and longitudinal arch. For example, plantar fasciitis is increasingly common in the later stages of pregnancy when rapid weight gain occurs over a short period, and relaxin hormone levels are elevated in the bloodstream, decreasing connective tissue strength.
Footwear and ground surface also plays an important role in cumulative trauma of the plantar fascia. Certain types of shoes, such as high-heeled shoes, decrease the shock-absorbing quality of the plantar fascia because they significantly alter foot mechanics. Likewise, steel-shanked construction boots decrease the foot’s flexibility and may lead to cumulative trauma, especially if the person walks or stands on a hard surface all day. Therefore, improper footwear and repetitive loading produce a double dilemma that may lead to plantar foot pain.
Nerve Entrapment in the Foot
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a nerve entrapment problem that produces pain and other neurological sensations on the bottom surface of the foot. Because of the pain location, it is commonly mistaken for plantar fasciitis. Like carpal tunnel syndrome in the wrist, it involves a nerve passing through a fibro-osseous tunnel created by a binding retinaculum.
The tibial nerve courses through the lower leg in the deep posterior compartment. As the nerve exits the deep posterior compartment, it passes around the medial side of the ankle on its way to the toes. Near the medial malleolus, the tibial nerve divides into three branches. The medial calcaneal nerve is primarily a sensory branch that serves the posterior and bottom surface of the heel. The other branches, the medial and lateral plantar nerves, carry motor and sensory signals to the plantar surface of the foot and into the toes.
Just after the tibial nerve divides into these three branches, they all pass under a fascial band on the medial side of the ankle called the flexor retinaculum or laciniate ligament (Image 2). The retinaculum is connected superiorly to the medial malleolus and inferiorly to the medial side of the calcaneus. This space under the retinaculum is the tarsal tunnel. In some people, the nerve branches after passing through the tunnel instead of before entering it. Several other structures pass through the tunnel, including the tendons of the tibialis posterior, flexor digitorum longus, flexor hallucis longus, and the posterior tibial artery and vein.

Image courtesy of Complete Anatomy
Tarsal tunnel syndrome results when compressive or tensile stress irritates the nerve in the tunnel. Compression can occur from extrinsic factors outside the tunnel, such as a direct blow to the medial side of the ankle or fractures or dislocations that compress the nerve. Nerve compression also occurs from intrinsic factors, such as inflammation, space-occupying lesions, or ganglions, which press on the nerve within the tunnel.
Tensile (pulling) forces on the nerves in the tarsal tunnel may also cause symptoms. Neural tension results from either a sudden stretch of the nerves or from biomechanical distortion, such as a calcaneal valgus foot alignment that stretches the nerves.
Peripheral neuropathies like tarsal tunnel syndrome are linked to diabetes, muscular sclerosis, rheumatoid arthritis, and hyperthyroidism. Some medications may cause sensitivity in the distal lower extremity nerves that could be mistaken for compression or tension pathologies in the tarsal tunnel.
Morton’s Neuroma
Morton’s neuroma is a nerve compression pathology involving the digital plantar nerves. The digital nerves are the terminal extension of the medial and lateral plantar nerves, which are divisions of the tibial branch of the sciatic nerve (Image 3).

Image courtesy of Complete Anatomy
The metatarsal heads are bound together by the deep and superficial transverse metatarsal ligaments, which create a small opening or tunnel between the metatarsal heads. The plantar digital nerve branches course through these small tunnels between the metatarsal heads.
The path of the plantar digital nerves between the superficial and deep transverse metatarsal ligaments is relatively narrow. At the same time, these nerves must pass between the metatarsal heads, making their tunnel of passage even smaller. While nerves can be compressed between any pair of metatarsal heads, the most common location for plantar digital nerve entrapment is between the third and fourth metatarsals. The space between these metatarsal heads is smaller than between any other pair.
Plantar digital nerve compression affects women more commonly than men. High-heeled shoes are one likely reason for that difference. When the heel is lifted higher than the forefoot, it essentially jams the foot into the front portion of the shoe, thus squeezing the metatarsal heads tightly together. Thus, compression increases on the nerves between the metatarsal heads.
Narrow-toe box shoes are a frequent contributor to plantar digital nerve compression. Any shoe with a narrow toe box can increase nerve compression by squeezing the metatarsal heads together. A narrow toe-box can occur in all types of shoes, from athletic to dress shoes, along with other shoes like cowboy boots.
Baxter’s Neuropathy
A potential cause of plantar foot pain often mistaken for plantar fasciitis is compression of the inferior calcaneal nerve (ICN) under the foot’s arch. The ICN is a branch of the lateral plantar nerve on the bottom surface of the foot. The nerve is also sometimes called Baxter’s nerve, named after the first physician to describe this nerve compression as a specific cause of foot pain. Compression pathology of this nerve is therefore called Baxter’s neuropathy.
As noted previously, the tibial nerve divides into two primary branches, the medial and lateral plantar nerves, as it passes around the medial side of the ankle in the tarsal tunnel. The first smaller branch that splits off from the lateral plantar nerve is the inferior calcaneal nerve (ICN) (Image 2- see if we can get this into image 2).
In Baxter’s neuropathy, there are two potential locations of entrapment of the ICN. The first is between the deep fascia of the abductor hallucis muscle and the quadratus plantae muscle. The second is along the medial calcaneal tuberosity, where the nerve can be compressed against the bone or bone spurs that may have developed along the anterior calcaneus due to plantar fasciitis or some other cause.
Muscle-Tendon Pathology
Another potential source of plantar foot pain is strain, trigger points, or dysfunction in the muscles and tendons on the plantar surface of the foot. There are two broad categories of muscles to consider in this region: extrinsic and intrinsic. Extrinsic muscles originate outside of the foot and include the muscles of the deep posterior compartment that have tendons coursing under the bottom surface of the foot. These are the flexor hallucis longus (FHL), flexor digitorum longus (FDL), and tibialis posterior (TP) (Image 2). Intrinsic muscles have both ends of attachment within the foot complex. This group includes the interosseous and lumbrical muscles and the quadratus plantae (Image 4). Let’s take a look at these two muscle groups.
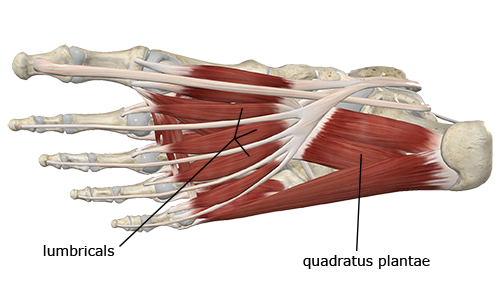
Image courtesy of Complete Anatomy
The Extrinsic Muscles
All three (FHL, FDL, & TP) muscles course around the medial side of the ankle as they pass under the flexor retinaculum in the tarsal tunnel (Image 2). One common cause of foot and ankle pain in these tendons is friction and irritation of the tendons in the tarsal tunnel.
In addition to tarsal tunnel irritation, problems may also occur with these tendons on the plantar surface of the foot. Scar tissue from tendon irritation or plantar fasciitis may cause the tendons to adhere to each other. Adhesion between these structures may be evident if there is a significant clawing of the other toes when the flexor hallucis longus is activated during attempted flexion of the great toe.
The Intrinsic Muscles
The intrinsic muscles are short muscles with both attachment points within the foot. As noted, this group includes the lumbricals, interosseous muscles, and quadratus plantae, among others. Because these muscles are so short, they aren’t often strained because their size doesn’t allow excessive lengthening while under contractile load. However, strains are possible in these muscles. A strain to one of these short intrinsic foot muscles could easily be mistaken for something more common, like plantar fasciitis or tarsal tunnel syndrome.
The foot is under extreme compressive loads, especially during repetitive lower extremity athletic activities like running and jumping. Improper footwear, lack of conditioning, excessive overuse, or numerous other factors could lead to hypertonicity or the development of myofascial trigger points that would produce plantar foot pain. Other factors, such as shoes with very high or deficient arch support, may alter foot biomechanics to the point that these muscles become painful due to overuse or trigger point development.
Conclusion
While these are not the only cause of plantar foot pain, they are some of the most common. As noted, plantar foot pain can be a debilitating problem, and clients will often seek your help in resolving this complaint. Luckily soft-tissue therapies like massage can play a significant role in reducing painful symptoms and returning to full function.
It is clear that learning more about specifc pathologies can greatly help you provide more effective care for your clients and get them back on their feet! That’s why our online orthopedic massage courses are structured around learning about individual conditions, how to evaluate them, and how to formulate an appropriate treatment strategy. Check out or Orthopedic Massage for the Foot, Ankle, & Leg course for deeper insights into conditions like those mentioned in the article and numerous others.

