Exploring Tendon Sheaths and Retinacula
- Whitney Lowe
One of the unique mechanical properties of our human structure is the presence of a retinaculum (plural: retinacula) around many of the joints of the body. A retinaculum is a band or membrane that holds an organ or part in its place. It may also be defined as a thickening of the deep fascia in distal portions of the limbs that hold tendons in positions when muscles contract.1 The structure of the retinacula in different regions of the body greatly aid mechanical function of the muscles and tendons acting on that region. Yet there are also some structural challenges with the retinacula that lead to a number of soft-tissue disorders.
Anatomical Structure
A retinaculum is composed of dense fibrous connective tissue that is an extension of the deep fascia. It often acts like a ligament in that it does not have contractile properties and may help with joint stability. Most of the retinacula in our body are found in the distal upper and lower extremities where they play a key role in helping generate forces for the muscles and tendons in this area. The function of the retinacula become much more apparent as we look at how they interact with tendons in the distal extremities.
Many tendons in the distal extremities are surrounded by a synovial sheath. The synovial sheath is one of two fibrous membranes that may cover the tendon. However, not every tendon has a synovial sheath. In fact, most tendons do not. The synovial sheaths are prevalent in those tendons of the distal extremities that course underneath a retinacula (Figure 1). The purpose of the tendon sheath, as we will explore below, is to reduce tension between the tendon and the binding retinaculum.
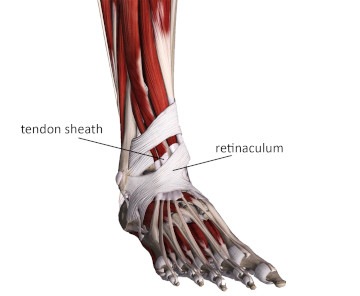
Figure 1
Synovial sheath under a retinacula
Image is from 3D4Medical’s Complete Anatomy application
Biomechanical Considerations
Most muscles have a relatively straight line of pull without any obstructions in their way. For example, the pectoralis minor pictured in Figure 2 has a short and straight line of pull between its attachment points on the coracoid process and the ribs with no significant angle to the tendon.
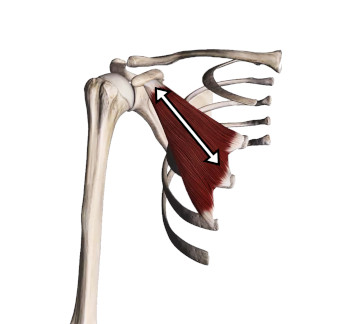
Figure 2
Straight line of pull of pectoralis minor
Image is from 3D4Medical’s Complete Anatomy application
The muscles of the distal extremities are different. In the long tendons of the hands and feet the tendons do not have a straight line of pull. In some instances the tendon must take almost a right angle turn. The long extensors of the toes pictured in Figure 3 are a good example. They travel the length of the lower leg and then over the top of the foot to the toes. They must make almost a 900 angle bend over the top of the foot near the ankle joint.
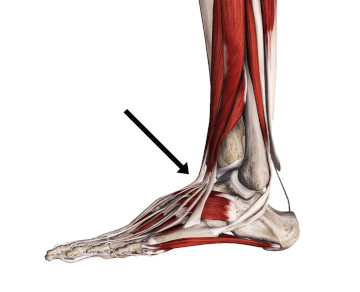
Figure 3
Lateral view of toe extensors showing significant bend in the tendon
Image is from 3D4Medical’s Complete Anatomy application
In order for these tendons to be mechanically efficient they must be held close to the joint. If they weren’t, the tendons would be pulled away from the joint when the muscle contracted and the muscle would lose its mechanical efficiency. The body creates a natural pulley- like structure with the retinaculum that improves the mechanical efficiency of the tendons by holding them close to the joint (Figure 4).

Figure 4
Natural pulley-like arrangement of the tendon and retinaculum
Image is from 3D4Medical’s Complete Anatomy application
By holding the tendons close to the joint, the binding retinaculum greatly improves the efficiency of the contraction force generated by the muscles and transmitted through the tendon. However, there is a potential downside to this arrangement as well. Holding the tendons close to the joint while they are trying to slide back and forth greatly increases friction between the tendon and the retinaculum. This excessive friction can lead to tendon damage.
The body has compensated for that potential problem by enclosing these vulnerable tendons in a synovial sheath. The tendons slide back and forth inside the synovial sheath and therefore do not rub against the binding retinaculum. If the synovial sheath were not present, the friction against the retinaculum would damage the tendon fibers.
Presence of the synovial sheath does not completely resolve the friction problem for these tendons that bend underneath a retinaculum. Sometimes repetitive motion or compression during movement will cause an irritation between the tendon and its surrounding synovial sheath. Fibrous adhesions or a roughening of the surface between the tendon and its sheath may develop. This condition is known as tenosynovitis.
There is a common tenosynovitis condition that develops over the top of the foot where the long extensors of the toes pass under the extensor retinaculum. If there is excessive compression of these tendons, tenosynovitis may develop. In this region it is commonly called “lace bite” because tight shoelaces are often the primary cause. Tenosynovitis is treated very similar to tendinitis. Deep friction massage over the affected tendon may help mobilize the tendon and reduce adhesions between the tendon and its sheath. However, activity modifications and reduction of tendon compression is crucial to fully resolve this problem.
Retinacula in the distal extremities also end up playing a prominent role in a number of other pathological conditions. When they span across joints they create space underneath that is occupied by tendons, arteries, veins, and nerves. The space underneath these retinacula are the soft-tissue tunnels that we commonly hear about, such as the carpal tunnel in the wrist or tarsal tunnel in the foot. Because the retinacular tissues is a dense fibrous connective tissue, it often produces an unyielding wall to the tunnel which can then lead to various nerve or vascular compression problems. Most well-known nerve compression problems are named for the retinacular tunnel where the nerve is getting squeezed.
When attempting to treat a nerve compression problem under the retinaculum, keep in mind that unlike muscle tissue, the retinacular tissue is not contractile tissue and does not “let go.” There is usually not a benefit in trying to work directly on the retinaculum to decrease the pathological nerve compression and further compression directly on this area may aggravate the condition. Treatment strategies need to focus on other methods to help reduce compression on the nerve within the tunnel. This usually means an emphasis on biomechanical change, reduction of offending activities, or both.
Most of the time a retinaculum is spanning the joints of the distal extremities to help produce mechanical advantage of the tendons. However, in other places the retinaculum has a different mechanical function. The quadriceps (or patellar) retinaculum is a very good example.
The quadriceps muscle group is large and has to generate very strong contraction forces across the knee during locomotion. Most anatomy references show the four quadriceps muscles blending into the patellar tendon. The patella is actually a floating bone that is embedded within the tendon.
However, there is a significant expanse of connective tissue from the distal quadriceps muscles that does not go directly into the patellar tendon. It does eventually connect with the proximal tibia and gives a much greater contact area for the quadriceps connections (Figure 5). This expanse of connective tissue on both sides of the knee is the patellar (or quadriceps) retinaculum and it serves to spread out some of the contractile force of the quadriceps and decrease the overall load on the patellar tendon.
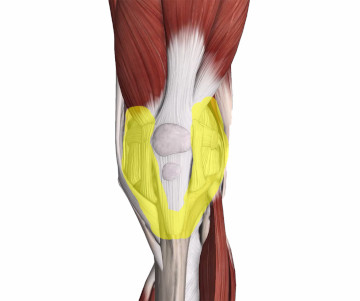
Figure 5
Patellar retinaculum (highlighted in yellow) helps transmit contractile forces from the quadriceps to the tibia
Image is from 3D4Medical’s Complete Anatomy application
An important consideration of the patellar retinaculum is that these tissues are richly innervated. The rich innervation of the patellar retinaculum plays a part in another common problem affecting the knee region called patellofemoral pain syndrome. And imbalance of forces between the quadriceps muscles can cause the patella to be pulled more to one side (usually laterally) during movement. When the patella is pulled more to one side there is excessive tension on the retinacular fibers of the opposite side as they are attempting to offset those forces. Excess tension on the retinacular tissues is likely the cause of pain in many patellofemoral pain conditions.
Massage therapy can be an effective method to address the anterior knee pain and tracking disorders affecting the patellar retinaculum. Deep stripping applications applied directly to the patellar retinaculum, especially during active movement are particularly helpful. It is also very important to work the entire length of the quadricep muscle group as these powerful muscles are the ones that are pulling on the retinacular fibers.
The retinacula and their associated tendon sheaths play a crucial role in the mechanics of our distal extremities. The significant range of motion we have at these joints where tendons must bend at very sharp angles poses serious mechanical challenges and often leads to overuse tendon disorders. It is very helpful when we understand the mechanical demands placed on these tissues and how our soft-tissue work can help them operate as efficiently as possible. If you want to see a more thorough visual description of tendon sheaths and retinacula, make sure to check out this video: http://bit.ly/2jIPHyp.

