Hooked on Shoulder Pain
- Whitney Lowe
Introduction
We tend to look at anatomy and structure as something that is constant and unchanging, but the truth is there are a number of anatomical variations and many of the structures shown in anatomy books can be somewhat different among individuals. Adding to this complexity, a client’s anatomical structure can significantly change with age, and those alterations can be the source for numerous soft-tissue pathologies. In this installment we’ll take a tour of subacromial architecture in the shoulder and explore how it differs between individuals and alters over time. These are critical factors to consider when determining the cause of shoulder pathologies.
The Architecture
The glenohumeral joint has the greatest range of motion of any joint in the body. The structure of the joint is such that there is very little stability provided by the bony architecture. As a result, the soft-tissues in this joint play a very important role in managing movement and providing stability.
One of the most common regions for soft-tissue injury in the shoulder is the subacromial space, so let’s take a more detailed look at the structures in and around this region. The subacromial space, as the name suggests, is the region under the acromion process. Problems are most common directly under the acromion process, but may also occur in nearby areas that not directly under the acromion.
The coracoacromial arch (Figure 1) is a key area for soft-tissue injuries around the shoulder. The arch is created by the acromion process, the coracoid process, and the coracoacromial ligament which joins these two bony projections. The coracoacromial ligament is somewhat unique as ligament structures go as most ligaments span from one bone to another in order to improve structural stability. The coracoacromial ligament spans between two projections of the same bone so it never moves or changes length as do most other ligaments.
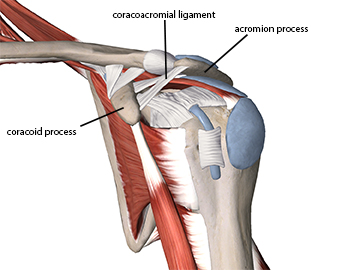
Figure 1
The Coracoacromial Arch
A number of soft-tissue structures can become compressed under the coracoacromial arch, including the supraspinatus muscle and tendon, biceps brachii long head tendon, subacromial bursa, glenohumeral joint capsule, subscapularis tendon, and coracohumeral ligament. These structures can be compressed under different regions of the coracoacromial arch.
One key factor that plays an important role in the likelihood of subacromial impingement is the shape of the acromion process. Anatomy books tend to show the acromion process as relatively flat, but other anatomic variations are common. The most common classification for differing shapes of the acromion is that originally described by Bigliani, shown in Figure 2.1
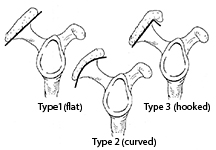
Figure 2
Three types of acromion process
Bigliani classifies three different shapes of the acromion process. The most common is the Type 1 or flat acromion in which the underside of the acromion is relatively flat. The Type 2 or curved acromion has a curved shape which is concave on the inferior side of the acromion. It is the Type 3 or “hooked” acromion that warrants special attention in many subacromial impingement problems.
The structure and shape of the acromion can vary from person to person, but one of the more interesting factors of the acromion shape variations is that they can change. Most notably a Type 1 or 2 acromion can eventually become a Type 3, hooked acromion. So how does the shape of this bone change?
Various structures in the body change shape or form as we age. For example, the intervertebral discs lose height and the spine gradually compresses as we age, thus older people become shorter. The acromion’s shape changes in reaction to mechanical and physiological forces acting on the structures that attach to it.
The coracoacromial ligament spans between the coracoid and acromion processes of the scapula. Tensile forces transmitted through the coracoacromial ligament pull on its attachment site at the acromion process. The body often develops calcification in regions where the bone is stressed as it perceives a bony injury. Calcification occurs at this attachment site in reaction to the constant pulling of the ligament as its fibers blend through the periosteum and into the bone. Over time the buildup of calcification causes the hook to develop on the end of the acromion.
Bone spurs can also develop on the underside of the acromion process, usually from the humeral head repeatedly impacting the underside of the acromion process. In either case the hooked acromion results from forces impacting the acromion process over time. These calcifications don’t happen quickly and that is why it is not common to see the hooked acromion in young people.
The hooked acromion is a frequent contributor to soft-tissue disorders such as subacromial bursitis, shoulder impingement, and rotator cuff dysfunction. The hook on the end of the acromion takes up crucial subacromial space and causes increased friction on a number of soft-tissues that lie under the acromion. The size of the hook may or may not be relevant to the level of damage, or the client’s individual experience of the pain. Even a relatively small hook can sometimes be enough to create dysfunction and pain for the client.
Now that you have a clearer picture of structural variations in the acromion process you may wonder why it matters and how it affects your massage practice. Shoulder pain is a very common reason for people to seek help from a massage therapist. Massage is often advocated for shoulder pain because there are so many soft-tissues in this region. When soft-tissue injury or dysfunction results from a hooked acromion, the root of the problem and the condition will recur until that dysfunctional structure is addressed. Massage can, however, be helpful in addressing some of the shoulder pain that occurs.
In a case where it is possible that a hooked acromion is aggravating the client’s condition it is advisable that the client be referred to an orthopedist (who specializes in shoulder injuries) to determine if surgery is warranted. The arthroscopic shoulder procedures for addressing subacromial morphology have advanced greatly and are generally minimally invasive, with recovery times much shorter than they were previously. The client should be aware that the continued impairment of soft-tissues under a hooked acromion can lead to longer and more involved damage and disability.
So if you have a client that is experiencing shoulder pain, pay close attention to the location of pain and what motions or activities aggravate that pain. If the pain is felt in the anterior or lateral shoulder region and aggravated with forward flexion or abduction, there is a good chance that subacromial pathology of some kind exists. If the client is over 30 there is an increasing chance that a hooked acromion could be involved. The older they are, the greater is the chance of this shape variation. You may not be able to accurately palpate the hooked acromion so it is best to refer them to another health professional for a comprehensive evaluation.
Resources
1. Balke M, Schmidt C, Dedy N, Banerjee M, Bouillon B, Liem D. Correlation of acromial morphology with impingement syndrome and rotator cuff tears. Acta Orthop. 2013;84(2):178-83.

