Is That A Supraspinatus Or Subscapularis Issue?
- Whitney Lowe
Introduction
Rotator cuff pathology is one of the most common causes of shoulder pain. However, it is common for someone to get a diagnosis of a rotator cuff tear or dysfunction without specifying which rotator cuff muscle(s) is/are involved. The rotator cuff comprises four muscles: supraspinatus, infraspinatus, teres minor, and subscapularis. These muscles are regularly implicated in shoulder complaints.
The supraspinatus and subscapularis are frequently involved in shoulder complaints. Because of their proximity and coordinated function, it may be difficult to unravel their role. Let’s look at some similarities and differences in signs and symptoms when they are involved.
Similar symptoms
One of the challenges with the supraspinatus and subscapularis muscles is they often share similar signs and symptoms for certain shoulder pathologies. Here is a short list of what may occur when either muscle (or possibly both) is/are affected:
- Anterior/lateral shoulder pain
- Pain with active or passive flexion
- History of repetitive overuse
- Pain with resisted abduction or resisted flexion
- Pain with active or passive shoulder abduction
The architecture of the subacromial region is a primary factor leading to injuries with both of these muscles. They both course under a region called the coracoacromial arch. This arch is comprised of the acromion process, coracoid process, and coracoacromial ligament that spans between them (Image 1).
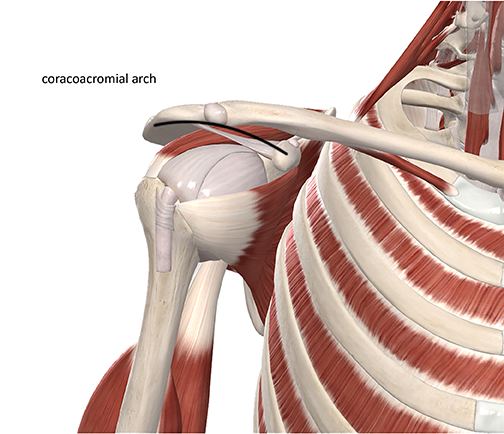
The coracoacromial arch
Image Courtesy of Complete Anatomy
Various shoulder motions may cause the supraspinatus or subscapularis to get pinched or compressed against adjacent structures under the coracoacromial arch.
However, a few important evaluation procedures can help you distinguish between supraspinatus and subscapularis involvement in certain shoulder complaints. Applying your knowledge of anatomy and shoulder mechanics will go a long way to assist you in making some of these distinctions.
One of the first places to begin is with palpation. While these muscles are close together, there are regions where they are distinctly separate, and palpating each will identify if the pain is reproduced from that particular muscle. Unfortunately, much of the supraspinatus is inaccessible under the acromion process, and much of the subscapularis is inaccessible on the anterior face of the scapula. However, using palpation in combination with other evaluation procedures mentioned below can create a more complete picture of the muscle’s potential involvement.
If the assessment procedures below produce the pain of the complaint, there is a greater likelihood that the particular muscle is involved. Keep in mind that no evaluation procedure can guarantee that any specific tissue will be involved.
The evaluation procedures listed below focus on muscle-tendon pathologies in which there is a biological or biomechanical dysfunction in the muscle (muscle strain, compression pathology, etc.) There are pain conditions in which additional factors play a primary role. These other factors are not identified through the evaluation procedures listed below. However, using these physical examination procedures can be very beneficial in narrowing down potential soft-tissue issues.
Subscapularis
Resisted medial rotation: Medial rotation is the primary action of the subscapularis when engaged in a concentric contraction. Resisting medial rotation recruits the muscle-tendon unit. Engaging this contraction will likely reproduce the client’s primary pain if there is injury or damage to that muscle-tendon unit. The supraspinatus is not significantly engaged during the resisted medial rotation. If this reproduces pain, it is more likely to involve the subscapularis.
Passive lateral rotation: The subscapularis is stretched during passive lateral rotation. There is minimal load on the supraspinatus during lateral rotation, so if this action reproduces pain, it is more likely an indicator of subscapularis involvement and not supraspinatus.
The above evaluation procedures can be more accurate if the distal portion of the subscapularis tendon is palpated during the manual resistive test or passive stretch.
Supraspinatus
Resisted abduction: You can apply a resisted abduction test to determine if there is a greater likelihood of supraspinatus involvement compared to the subscapularis. The primary supraspinatus action is to initiate shoulder abduction. Resisting abduction engages the supraspinatus and does not recruit much activity in the subscapularis. If this motion increases pain, the supraspinatus is implicated.
To isolate supraspinatus activity further, you can vary the resisted abduction test. The manual resistive test described above is usually performed with the arm at about 45° of abduction. You can increase the test’s sensitivity by putting a more significant load on the supraspinatus. In the variation, bring the client’s arm into about 90° of abduction while instructing them to hold the position. Downward pressure can then be applied to the distal upper extremity to evaluate if it reproduces the client’s pain. If it does, the supraspinatus is likely involved. This position is the same as that used in the special orthopedic test called the drop arm test. Applying pressure to the distal supraspinatus tendon during either test above increases the sensitivity.
The supraspinatus is not easy to stretch. So, evaluation tests that emphasize stretching are less effective in indicating supraspinatus involvement.
Conclusion
Treatment will produce the best results if it is specific and targeted. Identifying when these muscles are involved will help you provide specific care to clients with shoulder pain. Effective care will allow your client to return to pain-free movement quickly and efficiently. In addition, home care and movement rehabilitation suggestions are more effective if you know which tissues to target. However, remember that other soft tissues in this region may be involved. A more detailed assessment would be required to investigate the role of these other soft tissues.
Want some more help identifying what type of soft-tissue pathology you are dealing with? Grab a copy of our Assessment Cheat Sheet and keep it handy in your treatment room. It will help you zero in on your client’s complaint and greatly improve your treatment success!

