Current Concepts in Sacroiliac Joint Dysfunction
- Whitney Lowe
The sacroiliac (SI) joint is one of the most interesting joints in the body. There actually isn’t a single sacroiliac joint, but rather a left and right SI joint. This joint is the articulation on the posterior side of the pelvis between the sacrum and the ilium. The sacrum is essentially a wedge held in place within the pelvic ring to provide stability and allow for a slight degree of movement. Because of the way humans have evolved to an upright standing posture, the SI joint has become far more important for weight distribution and mechanics between the upper and lower body. Let’s look at some of the more interesting aspects of structure and function of this unique joint.
In children and young adults the contact surface between the sacrum and ilium is rather smooth and the joint acts like a typical synovial joint. The smooth articular surface and corresponding joint capsule allow for a small amount of movement. As the individual moves into adulthood, the joint surfaces change significantly. The surface of the ilium and sacrum develop ridges and depressions that fit together more like puzzle pieces. We can infer from this change that as a person ages stability in the sacroiliac joint becomes more important than mobility. By the eighth decade of life about 10% of the population actually have completely fused SI joints.1
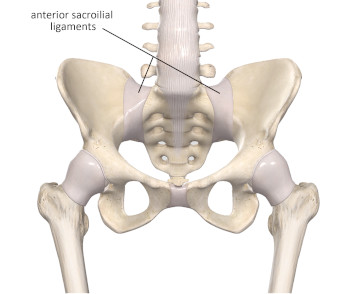
Image 1
Anterior sacroiliac ligaments
Image courtesy of Complete Anatomy
Stability at the SI joint is not only dependent on the contour surface between the adjacent bones, but is enhanced by a complex webbing of supporting and surrounding ligaments and other connective tissues. on the front side of the sacrum is the expanse of the anterior sacroiliac ligament complex (Image 1). There is a similar group of ligaments, the posterior sacroiliac ligaments, on the back side of the sacrum (Image 2).
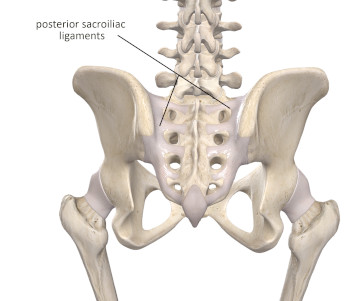
Image 2
Anterior sacroiliac ligaments
Image courtesy of Complete Anatomy
Additional sacral stability is provided by the sacrotuberous ligament (Image 3). It spans between the sacrum and the ischial tuberosity. There are fibrous expansions from the biceps femoris that go directly into the sacrotuberous ligament. These connections are important because tension throughout the hamstring muscle group can be transmitted to the sacrum through the sacrotuberous ligament. That connection provides a direct relationship of lower extremity mechanics to sacroiliac joint stability.
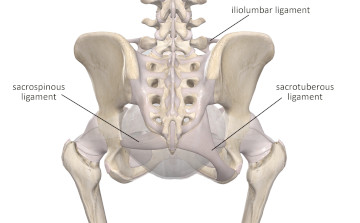
Image 3
Sacrotuberous, sacrospinous, and iliolumbar ligaments
Image courtesy of Complete Anatomy
The sacrospinous ligament which connects the sacrum with the ischial spine is another stabilizing force across the joint (Image 3). The iliolumbar ligament also contributes to stability at the SI joint (Image 3). This ligament spans between the transverse process of L5 (sometimes L4) and the posterior iliac crest. Some sources refer to the iliolumbar as the lumbosacral ligament.2
One of the more interesting facets contributing to stability of the sacroiliac joint has only come to light in recent years with the explorations of fascial anatomy. There are important fascial connections between muscles that span across the sacroiliac joint. For example, there is fascial continuity between the gluteus maximus on one side and latissimus dorsi on the other. There is also connection between the sacrotuberous ligament on one side and the gluteus maximus on that same side. These fascial connections seem to have an important role in force transmission across sacroiliac joint. What we are still discovering is to what extent we can influence force transmission across this joint with the manual therapy we apply to the soft tissues in the region. These myofascial connections across the sacroiliac joint are one of the main reasons why encouraging movement and strengthening of torso and lower extremity muscles play a crucial role in treatment of SI joint problems.
Pain in the lumbar, pelvic, or lower extremity regions is often attributed to problems of the SI joint. In most of these instances there is some alignment or movement disorder that is considered the root of the problem. However the more we are learning about biomechanics of the sacroiliac joint, the more some of these theories are called into question. Let’s take a deeper dive into some of the mechanics around the sacroiliac joint to understand this more thoroughly.
There is a slight degree of upward and downward sliding motion at the SI joint called translation. There is only about 1 to 2 mm worth of translation available at the SI joint, and this amount of movement will decrease if the person is older due to the increasingly complex contours between the sacrum and ilium. This amount of motion of the SI joint is almost inconsequential in most cases.
The majority of movement at the SI joint is a forward and backward tipping of the sacrum in relation to the ilium. This movement occurs around an imaginary horizontal axis going through the center of the sacrum. The forward movement of the sacrum in relation to the ilium is called nutation (Image 4). Keep in mind that the movement of nutation can occur when the sacrum tips forward, or when the ilium tips backward. The opposite of nutation is counternutation. In the counternutation movement, the top edge of the sacrum tips backward in relation to the ilium (Image 4). Counternutation can occur when the ilium tips backward or if the ilium tips forward in relation to the sacrum.
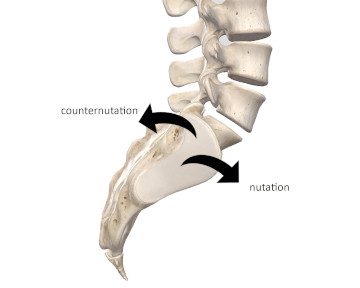
Image 4
Nutation and counternutation
Image courtesy of Complete Anatomy
There is only about 1-4° of movement capability in either nutation or counter nutation. That limited degree of movement at the SI joint has led to some common misunderstandings about SI joint mechanics. For example, as noted above if the ilium rotates anteriorly in relation to the sacrum, we would consider this a counternutation movement (it would essentially be the same as the sacrum tipping backward). However, if the SI joint only has less than 4° of movement, if there is more than about 4° of forward tipping, the ligaments become taut and the sacrum will be pulled into a forward tilt along with the ilia. So at this point the pelvis and sacrum are moving together and not independently. This may seem like a fine point of biomechanics, but it has a significant role in properly identifying dysfunctional movement at the sacroiliac joint that might be blamed for certain pain conditions.
Another important factor to investigate is the connection between mechanics in the lumbar region and those of the sacroiliac region. Because there is so little movement at the sacroiliac joint, the motion forces of the lumbar spine are transmitted through the sacroiliac joints to the pelvis. For example, if an individual has an exaggerated lumbar lordosis, forces from the lumbar region tip the sacrum in an anterior direction. Because the sacrum only has a few degrees of free movement in relation to the pelvis, these forces tip both the sacrum and pelvis in an anterior direction as well. With an anterior pelvic tilt the sacrum cannot disperse forces into the pelvis as effectively, and unequal loading at the SI joint may be contributing to pain in this region.
Sacroiliac Joint Dysfunction
Pain in the lumbar, gluteal, or lower extremity regions may arise from these dysfunctional mechanical loads or alignment problems at the SI joint and is referred to as sacroiliac joint dysfunction. This term should be considered a more general reference to motion or alignment problems and not a description of a specific tissue problem.
Symptoms of SI joint dysfunction include sharp or dull pain around the lumbosacral region. Sometimes it is difficult to precisely localize the point of pain. This pain may also be felt in the gluteal region, and can also mimic sciatic-type pain as it can travel down the posterior lower extremity as well.
Pain can arise from a sudden acute injury like a fall, but is more commonly associated with chronic postural problems or dysfunctional loading of the SI joint over long period of time. One example of long term unequal loading of the SI joints that contributes to pain in this region is either a functional or structural leg length discrepancy.
A functional leg length discrepancy occurs when muscles of the low back region, usually the quadratus lumborum, pull the pelvis higher on one side making it appear as if the leg is shorter on that side when the person is in a supine position. For example, if the right quadratus lumborum is hypertonic, it may pull the pelvis higher on the right side. When that individual is lying supine, it may appear as if the left leg is longer because the right side is being pulled higher (in a superior direction).
A true leg length discrepancy is one in which the bones of one lower extremity are actually longer than those on the other side. In this case the pelvis is pushed higher on the side with the longer leg (Image 5). In either event, the client will present with a lateral pelvic tilt and the transmission of forces from the lumbar region into the lower extremity through the sacroiliac joint will be unequally applied between sides and this may cause painful stresses on the joints.
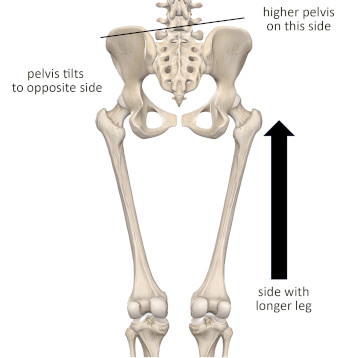
Image 5
Leg length discrepancy and SI joint dysfunction.
Longer leg produces higher pelvis on that side and tilt of pelvis to opposite side.
Image courtesy of Complete Anatomy
In the past, problems of the SI joint have frequently been ascribed to various postural challenges. Some of the problems like a leg length discrepancy described above are easier to identify. Other SI joint alignment problems can be more challenging to recognize through observation. Also remember that just because some apparent postural alignment challenge exists, like an anterior pelvic rotation, does not necessarily mean that there is a corresponding SI joint dysfunction or that it is the cause of your client’s pain.
SI joint dysfunction can produce tenderness in the soft tissues of the lower lumbar, gluteal, or upper sacral region. When palpated, active myofascial trigger points in the lumbar or gluteal regions can often reproduce the client’s pain as well. Despite pain or tenderness that might be felt in the area, lack of pain with palpation does not necessarily indicate absence of SI joint dysfunction. If pain is not reproduced with palpation, it could be because the irritated contact surfaces of the SI joint are not being reached. The anterior sacroiliac ligaments or the contact surface between the sacrum and ilium are examples regions not easily accessible to palpation.
Some clues about possible SI joint dysfunction may show up with basic range of motion evaluations in the hip and pelvis region. Pain may occur with several active motions of the hip or lumbar region including trunk flexion or extension, as well as hip flexion, abduction, or extension. In some cases pain occurs from adduction or rotational movements of the hip, but not often. In many cases the same motions may be uncomfortable with passive movement if the joint is stressed sufficiently. In other cases the role of muscles or gravity loading may make active movement painful when passive movement is not.
Due to the location of attachments of the lower lumbar erector spinae group in the SI region, pain may be felt with resisted extension of the lumbar spine. Due to fascial continuities in the region, pain could also be felt with resisted flexion, extension, lateral rotation, or abduction of the hip.
There are a number of special orthopedic tests designed to evaluate SI joint dysfunction. However, recent research studies have shown that none of these tests has a high degree of accuracy. Greater accuracy can be achieved when using several of them together, but clinicians are now moving away from focus on these evaluation procedures to identify SI joint problems.
Sacroiliac joint dysfunction is a primary problem of mechanical force loading at this complex joint. As a result, massage has limited direct impact on how those forces load the joint or how alignment of the joint can be adjusted. However, we also now recognize that pain complaints in any region of the body are not the simple result of alignment or mechanical problems in many cases. Rather, they may include complex issues of neural sensitization, fear of movement, mechanical stress, and a host of other factors that may all contribute to the existing complaint.
It is this complexity of factors that actually provides an opportunity for massage to be an effective intervention for SI joint pain. As we saw earlier, numerous muscles span the region and tension forces transmitted through myofascial tissues across this area may be contributing to the aggravating force loads. A wide variety of massage techniques applied to the lumbar gluteal and lower extremity regions can help reduce symptoms, help resolve dysfunctional mechanics, and contribute to improved functioning for our clients. There is no specific treatment protocol that is right for each client, and it is therefore important for the practitioner to identify what approaches decrease pain or discomfort to choose the most appropriate strategy.
- Neumann D. Kinesiology of the Musculoskeletal System. 34e ed. St. Louis: Mosby; 2016.
- Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537-567. doi:10.1111/j.1469-7580.2012.01564.x

