Shouldering the Challenge of Suprascapular Neuropathy
- Whitney Lowe
The shoulder is the most mobile joint in the body. The challenge with such extensive mobility, however, is that mechanical support and function relies heavily on the soft tissues. Consequently there are more soft-tissue disorders in this region. Bursitis and rotator cuff pathology are common diagnoses for soft-tissue shoulder pain. While both of these occur, other conditions can mimic these more common complaints. In situations like this treatment may be ineffective because they target the wrong cause. Damage or impairment to the suprascapular nerve can easily mimic a number of other shoulder complaints. Because of the location and function of this nerve, massage therapy can be a beneficial means of addressing suprascapular nerve disorders. Let’s take a look at the structure and function of this nerve, which often gets ignored in the evaluation and treatment process.
Anatomy
The suprascapular nerve is a relatively small and short nerve. Unfortunately it has to bypass several anatomical obstacles along its path and these obstacles are what make the nerve vulnerable to compression and tension injury. The suprascapular nerve originates from the C5 and C6 nerve roots and is a mixed nerve, meaning it carries both motor and sensory fibers. It provides sensory innervation to the posterior and lateral aspect of the shoulder and motor innervation to the supraspinatus and infraspinatus muscles.
The main portion of the nerve begins where it branches off of the superior trunk of the brachial plexus in the cervical region (Image 1). It branches off of the brachial plexus relatively high up along the bundle of nerves so it is less susceptible to a number of the other compression pathologies that affect lower portions of the brachial plexus.
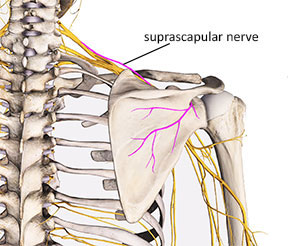
Image 1: Suprascapular nerve and its origin from brachial plexus
After branching off of the superior trunk of the brachial plexus it travels across the top of the shoulder on its way to the superior and lateral aspect of the scapula. The first primary anatomical obstacle it encounters is the narrow passage through the suprascapular notch (Image 2). The edges of the scapula along the suprascapular notch can be somewhat sharp and they may cause damage to the nerve when it is pulled taut against the edge of the notch.
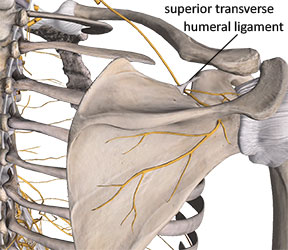
Image 2 Suprascapular notch with superior transverse ligament
There is a small ligament that spans the opening at the top of the suprascapular notch. This ligament is called the transverse scapular ligament. Because it spans the opening of the suprascapular notch it essentially creates a small foramen that the nerve must travel through (Image 2).
The transverse scapular ligament can sometimes become ossified, creating an even more rigid border for this narrow channel that the nerve passes through.1. There is also some indication that the suprascapular notch may narrow with aging. 2 Ligament ossification and narrowing of the opening at the suprascapular notch are both contributing factors to suprascapular nerve compression.
After the nerve courses through the suprascapular notch, branches extend out that innervate the supraspinatus muscle. Some of the remaining branches that pass the spine of the scapula and go down to the infraspinatus region may actually pass through the supraspinatus muscle; this is another potential site of nerve entrapment.
After passing the supraspinatus region, the nerve makes a sharp bend as it curves around the spinal glenoid notch (Image 3). Where the nerve bends around the rigid bony border of the spinoglenoid notch, it is vulnerable to compression.
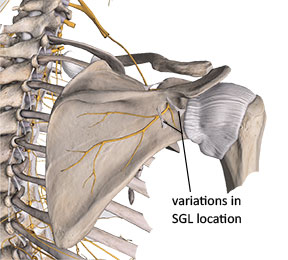
Image 3 Spinoglenoid notch and spinoglenoid ligament (SGL)
In up to 50% of people there is a connective tissue band called the spinoglenoid ligament that forms a second narrow tunnel where the nerve must pass (Image 3). 3 This ligament is also designated in some resources as the inferior transverse scapular ligament. Some anatomical references show this small ligament covering the suprascapular nerve farther along its path away from the spinoglenoid notch (Image 3). Because these small ligaments do not appear in all individuals, it is possible that there may be multiple locations where these anatomical anomalies occur. Regardless of their location, the impact on compressing the suprascapular nerve is similar in both situations.
Pathophysiology and Clinical Implications
Anatomical Considerations and Nerve Mechanics
The suprascapular nerve operates within a confined anatomical space, navigating between various structures around the shoulder. While nerves require some mobility to function properly, certain shoulder movements can place excessive mechanical stress on the suprascapular nerve. Understanding these mechanical relationships is crucial for proper assessment and treatment.
Movement-Related Stress Factors
Several common shoulder movements can create problematic nerve compression or tension:
Protraction and abduction pose particular challenges as they force the nerve against unyielding bony margins. Additionally, arm elevation and rotation can produce traction forces on the nerve through the movement of adjacent muscular structures. These mechanical stresses become especially relevant in occupations or activities requiring frequent overhead work.
Various shoulder pathologies may also compress or irritate the suprascapular nerve, including:
- Clavicular or scapular fractures
- Soft-tissue cysts or masses
- Rotator cuff tears
These conditions can alter the nerve’s normal pathway, leading to either compression or tension on the nerve fibers.
Clinical Implications and Movement Dysfunction
Suprascapular neuropathy creates a cascade of functional problems beyond just local nerve irritation. When the nerve is compressed, both the supraspinatus and infraspinatus muscles may atrophy, disrupting normal rotator cuff mechanics. This dysfunction particularly impacts movement control, such as during the deceleration phase of throwing motions.
For example, the infraspinatus and teres minor normally work together to control arm deceleration at the end of throwing. If nerve compression weakens the infraspinatus, it cannot generate sufficient eccentric force for proper deceleration. This weakness often leads to:
- Increased stress on the posterior capsular tissues
- Development of tendinosis in the remaining rotator cuff muscles
- Compensatory movement patterns that may create additional pathology
Clinical Presentation
Suprascapular neuropathy presents with both motor and sensory symptoms due to the nerve’s mixed fiber composition. Key clinical indicators include:
Motor Symptoms
- Muscle weakness, particularly in shoulder abduction and external rotation
- Visible muscle atrophy, especially in chronic cases
- Altered movement patterns during functional activities
Sensory Symptoms
- Posterior or lateral shoulder pain
- Altered sensation (numbness, tingling) in the affected region
- Pain exacerbation during specific movements
Identifying Suprascapular Neuropathy
Identifying suprascapular neuropathy presents unique clinical challenges because its symptoms often mirror other common shoulder conditions. For instance, lateral shoulder pain combined with difficulty in abduction frequently leads to initial diagnoses of rotator cuff pathology or subacromial bursitis. However, these same symptoms may indicate suprascapular nerve compression, where abduction difficulties stem from inadequate motor signals to the supraspinatus muscle, and pain occurs as the nerve experiences increasing tension during the movement.
Key Assessment Elements
Client History
The client history often provides crucial diagnostic clues. Watch for:
- Extended periods with the shoulder in abduction
- Repetitive movements involving shoulder abduction or protraction
- Sharp pain associated with specific positions
- History of overhead sports activities, particularly volleyball
- Occupational activities requiring sustained overhead work
Physical Observation
In advanced cases, careful observation of the posterior shoulder may reveal telling signs:
- Infraspinatus atrophy presents as a visible depression in the infraspinous fossa
- This atrophy is particularly notable because few other muscles overlay this region
- Asymmetry between shoulders often becomes apparent in unilateral cases
Muscle Testing
Resistive testing provides valuable information about nerve function:
- Always compare findings with the unaffected side
- Test resisted abduction to evaluate supraspinatus function
- Assess resisted external rotation to check infraspinatus integrity
- Remember that weakness rather than complete loss of function is typical, as other muscles can partially compensate for these movements
Pain Patterns and Nerve Relationships
Understanding pain referral patterns helps in diagnosis:
- Primary pain typically localizes to the posterior and lateral shoulder
- Some patients report pain radiating down the arm, following radial nerve distribution
- This radiation pattern relates to the shared neurological origins of the suprascapular and radial nerves (C5-C6 roots and superior trunk of brachial plexus)
Palpation Assessment
Careful palpation can help confirm nerve involvement:
- Check for sensitivity along the nerve’s anatomical path
- Test the distal region of the supraspinatus muscle
- Examine the lateral aspect of the infraspinatus near its musculotendinous junction
- Note that trigger points below the scapular spine often refer pain along the radial nerve distribution
- This referral pattern may relate to compression of the suprascapular nerve in this region
This comprehensive approach to assessment helps differentiate suprascapular neuropathy from other shoulder conditions, allowing for more targeted and effective treatment strategies. Understanding these assessment components enables practitioners to identify this often-overlooked condition and provide appropriate care or referral when necessary.
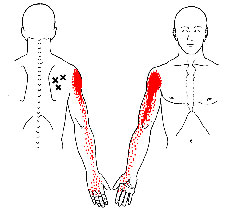
Image 4:
Common trigger points in the infraspinatus
Treatment
Suprascapular neuropathy can be a challenging problem to address because there are few things that can be done for it. The most important factor is to identify any biomechanical patterns, such as keeping the arms in abduction for long periods or excessive and repetitive motion that may be aggravating the nerve compression. Limiting those aggravating factors is the first strategy for addressing any nerve compression problem.
As noted earlier, branches of the suprascapular nerve may course directly through the supraspinatus muscle and may be bound or restricted by the other tissues that interface with the nerve. Consequently it is helpful to reduce any hypertonicity in the supraspinatus or infraspinatus muscles to encourage full freedom and mobility of the nerve so it can easily glide in relation to adjacent structures.
One of the most effective ways to help reduce hypertonicity in the supraspinatus muscle is through deep stripping techniques applied directly to the supraspinatus in a longitudinal direction along its length. It is difficult to access the most distal portion of the supraspinatus near its musculotendinous junction as the muscle goes under the acromion process at the acromioclavicular joint. However the area of potential suprascapular nerve restriction is more proximal to the region and is accessible through massage treatment.
When performing this stripping technique make sure the contact (finger, thumb, pressure tool) remains anterior to the large bundle of the upper trapezius. If you simply perform the stripping technique across the top of the shoulder without getting anterior to the trapezius you will simply be working on the trapezius and will give very little pressure down into the supraspinatus.
Once the contact point is established anterior to the trapezius, perform a slow longitudinal stripping technique along the length of the supraspinatus (Image 5). This can be performed moving medial to lateral or lateral to medial. One of the key goals of this longitudinal stripping technique is to help encourage mobility between the supraspinatus and the affected nerve. You can further enhance mobility by either actively or passively moving the client’s arm through abduction and adduction as you perform the stripping technique. Moving the muscle as you work on it helps increase greater tissue flexibility as well as mobility of all surrounding structures.
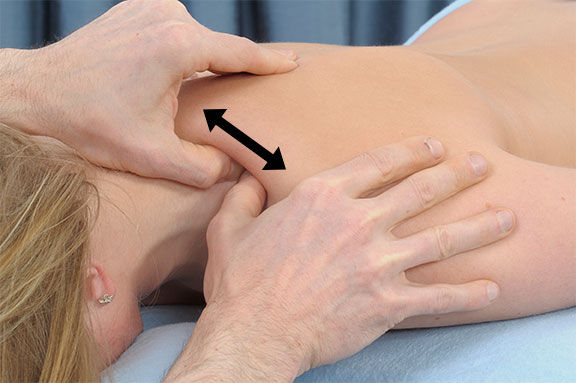
Image 5
Deep stripping to the supraspinatus
A similar technique can be applied to the infraspinatus to reduce hypertonicity and increase mobility between the suprascapular nerve and the infraspinatus muscle. With the client in a prone position, perform a slow stripping technique along the length of the infraspinatus muscle in a fan-shaped pattern with a small contact surface such as a finger, thumb, or pressure tool (Image 6). Make sure to check in with the client frequently about the appropriate depth of pressure and be sure not to apply so much pressure that any of the existing neurological sensations are increased. Be particularly cautious when applying pressure just inferior to the spine of the scapula, as that is where the primary area of nerve entrapment is usually located.

Image 6:
Deep stripping to the infraspinatus
Just like with the supraspinatus, it may be helpful to conduct active or passive movement during treatment to encourage full freedom of movement between the infraspinatus and suprascapular nerve. Often it is most effective to have the client moving the arm in medial rotation, so that the muscle is lengthening as the technique is applied. Make sure the client is close to the edge of the table to allow full freedom of movement through the entire range of motion in medial and lateral rotation as you apply this technique (Image 7).

Image 7:
Deep stripping to the infraspinatus during active medial rotation
While suprascapular neuropathy is not as common as other nerve compression problems like carpal tunnel syndrome, it is still valuable to know about its existence and recognize some of the key factors. It is particularly beneficial for massage therapists to be aware of this problem because there are few other treatment approaches that are as effective as massage in mobilizing the nearby tissues and helping the nerve’s return to optimum function. The massage therapist who is able to skillfully apply evaluation and treatment strategies for addressing this problem will be a valuable player in your client’s return to full function and health – and that means much more success for your practice!
References
- Pecina M, Markiewitz A, Krmpotic-Nemanic J. Tunnel Syndromes: Peripheral Nerve Compression Syndromes. Boca Raton: CRC Press; 2001.
- Yamakado K. The suprascapular notch narrows with aging: a preliminary solution of the old conjecture based on a 3D-CT evaluation. Surg Radiol Anat. 2016;38(6):693-697. doi:10.1007/s00276-015-1614-5.
- Kharay S, Sharma A, Singh P. Unusual morphology of scapulae: incidence and dimensions of ossified ligaments and supraspinous bony tunnels for clinical consideration. Singapore Med J. 2016;57(1):29-32. doi:10.11622/smedj.2015103.
- Witvrouw E, Cools A, Lysens R, et al. Suprascapular neuropathy in volleyball players. Br J Sports Med. 2000;34(3):174-180. http://www.ncbi.nlm.nih.gov/pubmed/10854016.

