Low Back Pain: Hidden Causes
- Whitney Lowe
Introduction
The human body is home to an extensive network of nerves that traverse nearly every tissue. The major nerves, like the sciatic, median, or ulnar nerves, are often the culprits in pathology. However, smaller nerves are also root causes of pain or injury complaints. These lesser-known nerves are frequently overlooked and lack extensive study. Some lie just under the skin, which means they can be affected by massage, either positively or negatively. In this post, we explore several of these important smaller nerves.
Dorsal Rami of Spinal Nerves
Recent research suggests that small nerve fibers, such as the dorsal rami, may significantly affect low back pain (Image 1). While low back pain can radiate into the lower extremities, it is often localized in the muscles and tissues nearest the spine—areas not innervated by the nerve branches extending into the lower extremities.
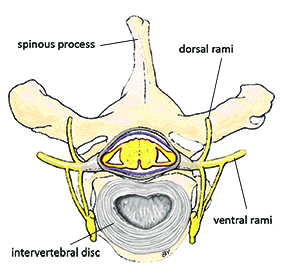
The dorsal rami are smaller nerve branches that emerge from the posterior aspect of the nerve root and are less vulnerable to disc compression than the ventral branches that make up the large lower extremity nerves. Dorsal rami are mixed nerves that carry both motor and sensory fibers. The motor fibers innervate the paraspinal muscles, such as the erector spinae group, and smaller intrinsic muscles, like the multifidus. Sensory fibers from the dorsal rami supply the skin along the spine and deep connective tissues of the vertebrae, including the posterior longitudinal ligament. Despite their size, dorsal rami can carry up to 200,000 nerve fibers, making them susceptible to causing pain from increased compression or tension.
Although the dorsal rami are relatively short and don’t travel through major anatomical structures like large bones or joints, they can still become restricted or pulled. This restriction can occur due to tension in nearby tissues, muscle tightness, or changes in posture or movement patterns. Many people experience pain in their paraspinal muscles (the muscles that run along the spine), which often worsens with direct pressure or stretching of these muscles. This discomfort may be linked to the sensory fibers of the dorsal rami, which supply sensation to the muscles and tissues in this region. When these fibers are irritated, they can contribute to the pain sensations individuals report.
Massage therapists can address paraspinal muscle pain using long gliding strokes along the length of the muscles. This technique helps reduce muscle tightness and increases blood flow to superficial capillaries and tissues that experience ischemia. Gentle approaches, such as myofascial release techniques, apply traction to the skin, reducing tensile forces on the dorsal rami nerve fibers. Noxious signals sent to the central nervous system are reduced by alleviating tension on these fibers, significantly diminishing back pain.
Inferior, Medial, & Superior Cluneal Nerves
Piriformis syndrome is often the first suspect in cases of severe gluteal pain. However, another set of superficial sensory nerves innervates the gluteal region—the inferior, medial, and superior cluneal nerves.
The cluneal nerves innervate superficial tissues throughout the entire gluteal region, yet they are rarely mentioned in pelvic or low back pain references. These sensory nerves, divided into three branches—inferior, medial, and superior (Image 2)—may be unfamiliar to many practitioners. The inferior division branches off the posterior femoral cutaneous nerve (PFCN) and can be affected by piriformis compression of the PFCN.
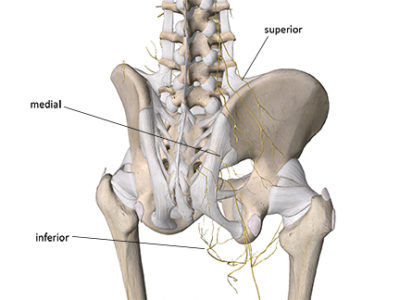
The medial cluneal nerve is derived from the dorsal branches of S1-S3 and innervates the skin over the middle buttock region. Other S1-S3 nerve roots supply innervation to the lower leg. Sometimes, sensory input from one region can spill over to adjacent nerve fibers derived from the same level. As a result, lower leg pain reported to the S1-S3 nerve roots can extend into the buttock region due to spillover to the medial cluneal nerves. Similarly, pain caused by entrapment of the medial cluneal nerves is likely to be felt in the buttock but may also be experienced in the lower leg.
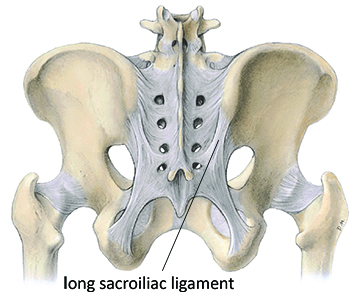
The medial cluneal nerve fibers pass adjacent to the long sacroiliac ligament, making this a vulnerable spot for compression (Image 3). Medial cluneal nerve Irritation or entrapment by the long posterior sacroiliac ligament is often mistaken for sacroiliac joint dysfunction. Assessing the possible tissues involved in sacroiliac joint pain is challenging because small nerves like the medial cluneal nerve might be involved.
The superior cluneal nerve is the branch most susceptible to compression injury and is a likely cause of back or gluteal pain. The pain from cluneal nerve entrapment is usually a bit more sharp and delineated that the more dull and generalized pain felt with many sacroiliac joint complaints. Its anatomical path reveals why it might be involved in these conditions (Image 4). The superior cluneal nerve arises from the posterior rami of the 1st through 3rd lumbar vertebrae and angles diagonally from the lumbar spine. Its branches pierce the thoracolumbar fascia and course across the upper margin of the iliac crest.
.
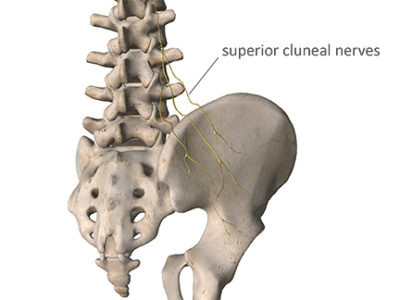
Superior cluneal nerve entrapment can occur as they pierce the thick thoracolumbar fascia or are compressed against the bony edge of the superior iliac crest. The thoracolumbar fascia is a dense fibrous tissue, making it difficult to increase its elasticity or pliability where the nerves pass through.
The region just under the lip of the iliac crest is a common location for small fatty lipomas, which feel like small peas under the skin during massage. I discuss these further in this post on back mice. While they don’t seem to involve significant tissue pathology, they can sometimes be painful. One possible explanation for this pain could be pressure on adjacent superior cluneal nerve fibers.
Since the cluneal nerves are superficial, they are easily affected during massage treatment on the gluteal region. Massage of the low back region can help improve superior cluneal nerve mobility in some cases. Techniques like static compression or broad contact sweeping reduce muscle tightness that may be involved in nerve entrapment.
The first step in resolving many clinical problems is assessing the tissues involved. Medical references often lack detailed coverage of these superficial nerves, so their dysfunctions can be easily overlooked. Understanding these structures’ functions might help you solve a client’s pain. Massage is highly beneficial for these conditions.
You can learn more about these and many other nerve compression challenges in our orthopedic medical massage courses. Head to our website at academyofclinicalmassage.com to continue your professional development and find effective solutions for your clients.
Notes
- Mixter, W J, and J S Barr. 1934. “Rupture of the Intervertebral Disc with Involvement of the Spinal Canal.” N Engl J Med 211: 210–15.
- Tubbs, RS, E Rizk, MM Shoja, M Loukas, N Barbaro, and R Spinner. 2015. Nerves and Nerve Injuries: Vol 1: History, Embryology, Anatomy, Imaging, and Diagnostics. Amsterdam: Elsevier.
- Aota, Yoichi. 2016. “Entrapment of Middle Cluneal Nerves as an Unknown Cause of Low Back Pain.” World Journal of Orthopedics 7 (3): 167–70. doi:10.5312/wjo.v7.i3.167.

