The Slump Test
- Whitney Lowe
Introduction
Physical examination provides crucial insights for locating potential nerve pathology, even when advanced diagnostic tests like nerve conduction studies prove inconclusive. The slump test stands out as one of the most effective methods for evaluating nerve compression and tension pathologies. This comprehensive neurodynamic test, first described by Australian physiotherapist Geoffrey Maitland, helps identify neural tissue involvement in various musculoskeletal conditions.
Test Development and Principles
The slump test evolved from Maitland’s clinical observation that certain positions could reproduce or exacerbate neurological symptoms. The test’s name derives from its primary position – a seated forward slump that places progressive tension on the neural structures. This systematic approach allows practitioners to assess the entire nerve tract from the cervical spine through the lower extremities.
Test Procedure
Initial Position
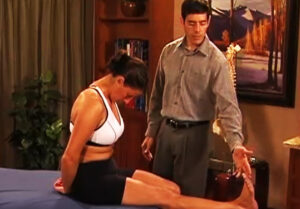
The slump test begins with precise client positioning. The client sits at the edge of the treatment table with their arms behind their back, establishing a stable base for the subsequent movements. This position allows for controlled application of neural tension through multiple body segments.
Upper Body Component
The first movement focuses on the upper body. The client slumps forward in the upper thoracic region while maintaining some head extension. The therapist may apply gentle overpressure to increase tension on the neural structures. This position specifically targets the cervical and upper thoracic neural tissues.
Cervical Component
With the thoracic slump maintained, the client slowly moves into full neck flexion. The therapist can provide additional overpressure to increase cervical flexion carefully. This step significantly increases tension in the cervical and upper thoracic neurological structures. Any symptoms in the upper extremity warrant careful attention, particularly if they follow specific dermatome or cutaneous nerve patterns.
Lower Extremity Integration
The test’s complexity increases with lower extremity involvement. The client actively extends their knee while maintaining the slumped position. This movement creates tensile stress on the sciatic nerve, which connects through the nerve roots to the dura mater and spinal cord. Even subtle tension at this stage can produce meaningful information.
Final Component
The final step involves ankle dorsiflexion with the knee maintained in extension. This movement further increases tension on the sciatic nerve and associated neural structures. The combination of all positions typically elicits increased neurological sensations along the nerve’s distribution if compression or tension exists anywhere in the tract.
Clinical Considerations
Not every client requires all test components. For example, if significant neurological symptoms appear during the upper thoracic slump and neck flexion, these findings alone may indicate sufficient neural involvement. Adding lower extremity movements might create excessive discomfort without providing additional diagnostic value. At any point in the process if significant neurological symptoms are created it is usually not required to continue through the other parts of the test because this can further aggravate the neurological symptoms.
Safety Precautions
The slump test requires careful application, particularly with certain pathologies. The slumped position can create substantial compressive forces on lumbar vertebrae, potentially affecting structures like the lumbar intervertebral discs or lumbar nerve roots. While identifying these issues is often the test’s purpose, practitioners must apply only necessary tension to avoid exacerbating the condition.
Significance in Assessment
The slump test provides valuable information about neural tension and pathology throughout the spinal canal and peripheral nerve tracts. Its systematic application helps practitioners identify the location and nature of neural involvement, guiding treatment decisions and monitoring progress. Understanding both the technique’s power and limitations ensures its effective use in clinical practice