Ulnar Nerve Entrapment
- Whitney Lowe
Introduction
Upper extremity nerve compression is a frequent concern for many clients and a painful condition that can cause serious work-related challenges. Understanding these problematic conditions is crucial. Carpal tunnel syndrome is the most common upper extremity neurological disorder, but ulnar nerve compression is more prevalent than realized. The ulnar nerve can be compressed in two main areas: at the elbow in the cubital tunnel, leading to cubital tunnel syndrome (CTS), and at the wrist in Guyon’s canal, resulting in Guyon’s canal syndrome (GCS).
Anatomical Background
The cubital tunnel, located at the back of the elbow, is formed by two separate heads of the flexor carpi ulnaris muscle (Image 1). The ulnar nerve runs through this tunnel, and its compression leads to cubital tunnel syndrome (CTS).
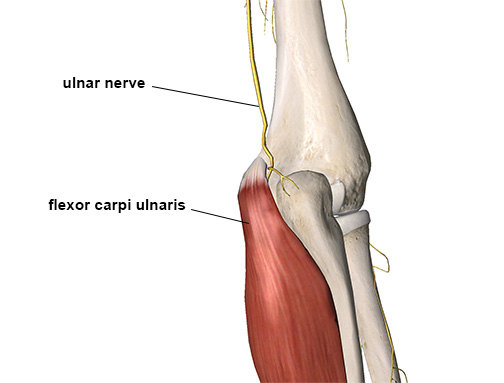
The ulnar nerve entering the cubital tunnel
CTS usually arises from prolonged low to moderate nerve pressure, often due to certain arm positions or fibrous bands in the muscle compressing the nerve. It is common in jobs requiring extended elbow flexion. Symptoms like hand numbness can occur from long periods of elbow bending, such as during sleep. Direct blows to the elbow can also cause CTS, but less frequently.
Guyon’s canal syndrome (GCS) differs from CTS. Located in the wrist near the carpal tunnel, Guyon’s canal houses the ulnar nerve, artery, and vein but does not contain any tendons (Image 2).
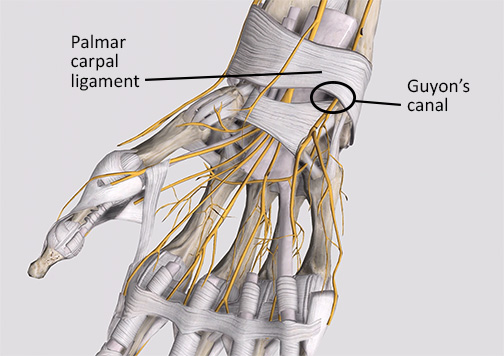
The ulnar nerve as it passes through Guyon’s canal in the wrist
In GCS, nerve compression isn’t due to tendon inflammation but other factors. Most GCS cases involve external pressure placed on the region from outside the body, like hitting something with the hand, as opposed to something that creates pressure inside the tunnel itself (such as the tendon inflammation of carpal tunnel syndrome).
GCS can be acute, often due to direct hand injuries when the wrist is bent back into extension, called a FOOSH injury, an acronym for Fall On Outstretched Hand. It may also occur as a chronic condition from prolonged pressure on the hand’s base. This disorder is common in long-distance cyclists and is known as ‘handlebar palsy.’
Assessment & Evaluation
Symptoms of ulnar nerve compression in CTS (Cubital Tunnel Syndrome) and GCS (Guyon’s Canal Syndrome) are often similar, including pain, numbness, or tingling in the hand’s ulnar nerve distribution (Image 3).
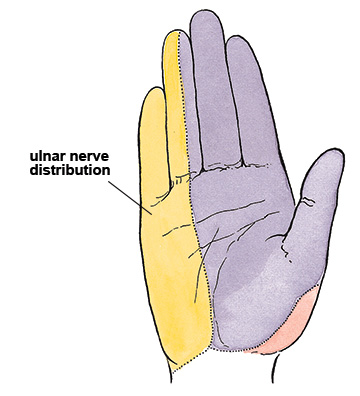
The area of the hand innervated by the ulnar nerve
It’s vital to confirm these symptoms are specific to the ulnar nerve, as they are commonly mistaken for carpal tunnel syndrome. CTS and GCS can cause weakness in ulnar nerve-controlled muscles, leading to difficulty gripping or precision tasks like writing.
Palpation can help you recognize both conditions. Applying pressure to the cubital tunnel in CTS or Guyon’s canal in GCS can reproduce neurological symptoms, so be careful with your pressure level during assessment and treatment.
Movement tests may also help in recognition. Each condition has a unique pattern of results with active, passive, and resisted movements. Recognizing these patterns is important in uncovering the presence of ulnar nerve compression. In our Elbow, Forearm, and Hand course, we demonstrate those patterns so you can learn to look for them.
Some special orthopedic tests may help recognize these conditions. For example, cubital tunnel compression symptoms may recur with sustained elbow flexion. Neurological symptoms may not occur by moving the elbow into flexion (like in a range of motion test). You may need to hold it in that position for a short period, like with a procedure called the elbow flexion test.
Treatment Strategies
Medical treatment for both CTS and GCS typically involves conservative methods like resting and using splints to minimize nerve irritation. Splints are particularly useful at night to prevent harmful wrist or elbow positions. Generally, once the nerve is no longer irritated, it heals naturally, although recovery can be slow.
In GCS, caused by external compression, reducing the pressure can suffice for treatment, but healing may take time. Nerve compression problems are notoriously slow to heal. For CTS, surgery might be considered if conservative approaches fail.
Massage has a limited role in GCS due to the risk of aggravating symptoms through further nerve compression. Avoid techniques that increase nerve compression, as indicated by worsening symptoms. However, massaging the entire upper extremity can be beneficial in reducing overall muscle tension to give the nerve the best chance to heal on its own.
CTS, which often results from muscular factors, may respond better to massage therapy. Focusing on reducing tension in the forearm’s flexor muscles, particularly the flexor carpi ulnaris, is key. To prevent exacerbating ulnar nerve compression, care is needed to avoid additional pressure over the cubital tunnel.
Conclusion
Upper extremity nerve compression issues, often caused by repetitive or prolonged upper extremity strain, can significantly impact the careers of massage therapists and others. Effective treatment hinges on accurately recognizing and targeting the main factors of a client’s condition. Your deepening knowledge and understanding of these issues will enhance your ability to successfully treat such complaints.

